By Lily Scheindlin
Congress’ January 18, 2023, decision to extend the continuing resolution (CR) staved off major cuts to federal healthcare spending. The CR was passed without changes to prior funding levels for most programs and keeps government programs operating until early March. The CR keeps the government funded through March 8, 2024. What can we anticipate next?
The continuing resolution and decisions on the federal budget have widespread implications to all areas of the nation, particularly on the public health system. Public health departments, hospitals, and healthcare facilities rely on key federal investments to make services available for all Americans and prepare long-term efforts and necessary planning for the future.
The CR keeps funding at current levels and halts any increase in funding for public health and public health programs. The CR expires on March 8, 2024, with the threat of a government shutdown if law makers do not agree on a budget to fund the government. A funding reduction could impact many public health programs and services, making access to healthcare difficult for all Americans, particularly those historically medically underserved.
Public health and healthcare leaders are concerned that possible funding reductions could negatively impact patients and vulnerable communities:
- Risk to state funding: Without consensus on budget appropriations, public health and emergency preparedness and response funding may not be adequate.
- Chronic underfunding in public health: Public health emergency response funding has traditionally been reactionary. Underinvestment in public health can lead to unpredictable allocations of resources in a response. As seen in disease outbreaks like H1N1, COVID-19, and Mpox, only after an emergency is declared are federal funds released. Millions of dollars of unspent COVID-19 funds are threatened to be clawed back, which would prevent states and jurisdictions from accessing funds that are still necessary for recovery and rebuilding infrastructure.
- Healthcare supply chain, already fragile, will suffer: Relationships to strengthen the supply chain were in part developed with funding that supported partnership between private sector stakeholders and hospital/public health systems. Rescission of COVID-19 funds threatens the progress made in advancing nimbleness across the healthcare supply chain.
- Threatens policies and programs: Funding allocations for policies that support the healthcare workforce and public health are up for reallocation, meaning that programs such as the National Health Service Corps and Teaching Health Center Graduate Medical Education may be lose funding.
More investment in public health needed
Cuts to current funding levels threaten the health of vulnerable populations. It is critical to work in unison to strengthen investments in US healthcare and public health to improve health outcomes and quality of life.
Healthcare Ready will continue to monitor federal budget talks. Regardless of the outcome, Healthcare Ready is committed to coordinating public and private partners, including federal agencies involved in disaster response, state emergency operations centers, and health systems — hospitals, clinics, and Federally Qualified Health Centers (FQHCs) — to assess healthcare needs and impacts by:
- Connecting needs and resources between nongovernmental organizations (NGOs), nonprofits, and shelters for supplies/medicines, and donations,
- Assessing potential risks to critical infrastructure and healthcare supply chains,
- Sharing resources and state-specific information to assist healthcare facilities, communities, and individuals,
- Intelligence gathering and situational reporting.
Lack of informed decision-making comes at a price
Effectively investing in preparedness requires information that can guide meaningful conversations about complex issues affecting the public health care sector. Unfortunately, many budget and policy decisions may be made without considering the full scope of the situation, overlooking the needs of underserved communities. In connecting needs and resources, Healthcare Ready’s intelligence gathering provides reports and policy briefs that are catalysts for change through evidence-based recommendations.
Our recent work includes a philanthropic-funded study highlighting the crucial role of community health centers, research data about the views of Americans regarding funding increases for disaster preparedness, and a report to Congress with recommendations to ensure our nation is prepared and equipped to respond to the next public health emergency.
Restoring the Healthcare Workforce for Equity Project: Healthcare Ready highlights threats to community health centers
A new Healthcare Ready study highlighted funding and policy issues facing community health centers. These centers play a vital role in addressing health disparities, providing comprehensive primary healthcare to medically underserved rural and urban communities and populations.
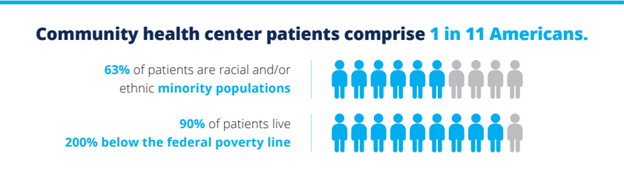
Each year, more than 31.5 million patients receive care from among more than 14,000 community health center locations operating across the U.S. Health centers serve diverse communities, and often are battling years of structural racism, while at the same time providing low-cost, high-quality care to community members.
Healthcare Ready’s study “Restoring the Healthcare Workforce for Equity Project” noted the various barriers to health center disaster preparedness, especially where public health is a concern. Funding of health centers is usually limited and specific to the event at hand even if centers received some funding for federally declared disasters. Examples of key barriers health centers face, limiting their capacity for preparedness and response and making it more difficult for communities to navigate recovery following a disaster, include:
- Limited resources
- Operational efficiency
- Limited supplies
- Geographic challenges
Protecting National Public Health and Health Care Infrastructure for the Next Disaster:
At the beginning of 2023, Healthcare Ready released a report to Congress calling for greater federal oversight, and increased communication, coordination, and preparedness among those responsible for organizing and responding to public health emergencies. The report, Protecting National Public Health and Health Care Infrastructure for the Next Disaster, made specific, straightforward recommendations to Congress and federal agencies to help ensure that the nation is prepared and equipped to respond to the next public health emergency. The four key takeaways are:
1) Improve communication and coordination across all stakeholders in preparedness and response, including public and private sector entities; federal agencies involved in health care preparedness and response; and federally funded programs and/or offices and recipients (or subrecipients) of federal cooperative agreements.
2) Strengthen accountability by setting targets for all program goals and benchmarks for all standards of Administration for Strategic Preparedness and Response (ASPR) Hospital Preparedness Program (HPP) Cooperative Agreements and Centers for Disease Control and Prevention Public Health Emergency Preparedness Cooperative Agreements; and ensure monitoring and evaluation of progress with transparent reporting of results.
3) Strengthen efforts to apply an equity lens to public health and health care preparedness and response by enhancing community engagement; addressing health-related social needs; and conducting research that will build the capacity of resources that support individuals with access and functional needs.
4) Increase funding for federal preparedness and response to strengthen national and regional capabilities, help to achieve better outcomes after disasters, and contribute to ensuring our nation’s health security against future public health threats.
This report was undertaken by Healthcare Ready as part of a cooperative agreement with ASPR, as required by Section 210 of the Pandemic and All-Hazards Preparedness and Advancing Innovation Act of 2019 (PAHPAIA) Public Law No. 116-22.
Implementation of the recommendations in this report will help to build public will for a strong preparedness system, create more effective and efficient preparedness systems and, importantly, help us meet the needs of all Americans — especially populations that are at greater risk of being disproportionately affected by disasters.
Finally…what if we head toward a government shutdown?
As we focus on recovering from the COVID-19 pandemic and prioritizing the current and future health of communities, adequate funding for public health initiatives is critical. As noted in our blog last September, a government shutdown, even a partial one, may have implications for healthcare delivery and disaster response. While most essential operations would be expected to continue, an extended shutdown could critically impact an array of programs. The effectiveness of the national response to emergencies relies heavily on established relationships across various sectors. A disruption of funding may compromise the intended rapid response structure of these networks, potentially impeding coordination, and delivery of vital services during emergencies. Maintaining the continuity of these programs is paramount to ensuring a robust, coordinated, and efficient healthcare response in times of crisis.