mAbs Treatment: Minimizing Hurdles and Why Accessibility Matters
Last month we wrote about monoclonal antibody treatments (mAbs) and the critical role they play in preventing hospitalizations amid the constantly shifting COVID-19 landscape of variants and hot spots. Most recently, we’re learning where mAbs are most effective given rising rates of variants in particular regions. In areas, such as Illinois and Massachusetts, the FDA recommends the use of REGEN-CoV over other available mAbs because of sustained reactivity against the P.1 variant (originally identified in Brazil), which has higher prevalence in those states.
Overall, the potential impact of mAbs in the battle against COVID-19 remains significant. mAbs have been shown to reduce the relative risk of hospitalizations or death by 70% in Phase 3 clinical trials. So, if the treatment works well, you might ask next: How much does it cost?
The federal government is paying for the product (i.e., the drug itself), making it free for all patients regardless of health insurance and immigration status. Administration of the treatment is free for Medicare patients, those who are uninsured, and for many on Medicaid or private insurance.
What else do patients, providers, and loved ones need to know about this critical COVID-19 treatment before they get sick?
Patients need the following in order to get treated for COVID-19:
- A positive test for COVD-19;
- A prescription from a provider for mAbs treatment; and
- An appointment with an infusion center for treatment within the first 10 days of symptom onset.
What can providers and health stakeholders do to minimize patient hurdles to timely access to mAbs?
- Providers and other public health stakeholders can play a key role in promoting the availability, safety, and efficacy of mAbs treatment for COVID-19.
- Inform patients of their options for COVID-19 treatment before they are diagnosed so they can act quickly if they get a positive diagnosis.
- Make it easy for a patient to get a prescription from a provider. Telehealth can be one option to bypass delays that may be caused by an in-person appointment.
- For patients without a primary care provider or who are unable to seek help at an urgent care center or emergency department, help navigate access to a provider at a local community health center.
- A provider that prescribes mAbs treatment (or, office staff) can help patients find an infusion center nearby and schedule an infusion appointment on their behalf.
Why does mAbs treatment accessibility matter?
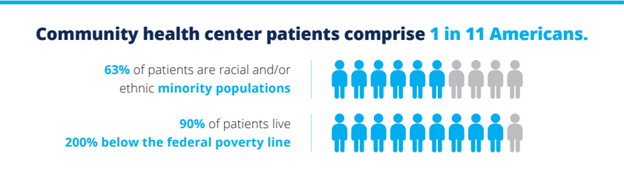
The disproportionate risk and impact on communities of color from the COVID-19 pandemic has brought long-standing issues of systemic health and social inequities to the forefront of conversations on problems with our healthcare system. Given the higher rates of infection, hospitalization, and death from COVID-19 among communities of color – Asians, Latin-X, Black, and Indigenous peoples – administration of treatments such as mAbs can be considered a racial equity issue as much as it is a healthcare issue alone.
mAbs in the treatment of COVID-19 can be a critical means for preventing the most severe outcomes for populations that have been hardest hit from the pandemic. Learn more about mAbs treatment here and find ways you can contribute to building the conversation to save lives and foster hope in the recovery from COVID-19.
With vaccinations rolling out and COVID-19 restrictions slowly reversing, most colleges are anticipating a full reopening and reintegration of students to campus. While the desire to “return to normal” may be universal, plans to reopen are far from uniform across the country.