As we enter the fall of 2023, pediatric healthcare faces a daunting challenge, with the convergence of three significant health crises — RSV, influenza, and COVID-19. This “tripledemic” poses unique threats to our children, exposing longstanding weaknesses in our healthcare infrastructure that must be urgently addressed.
In pediatric hospitals across the nation, a concerning issue looms large. Despite years of warnings, many emergency departments remain ill-equipped to handle pediatric cases. Only about 14% of these departments are certified to treat children, and most doctors lack the necessary experience to care for young patients. This deficiency is perpetuated by an alarming shortage of child-sized equipment and a default to adult drug doses and protocols when treating children. The consequences of this unpreparedness are severe. Countless avoidable child deaths and long-term health issues occur due to the lack of staff, appropriate supplies, and pediatric training.
Federal funding for pediatric emergency care is limited, and the financial incentive for hospitals to prioritize children’s health over adults’ is lacking. Safety standards are primarily geared toward all ages, with few specific pediatric-focused requirements.
The reality is that we continue to allow the well-being of our children to be compromised due to the lack of comprehensive regulations and incentives for improvement. It’s time for a change.
RSV
The 2022 RSV season revealed the devastating impact of RSV lower respiratory tract infections on infants in pediatric hospitals. Many of these infants were otherwise healthy, born at term, and yet, they suffered greatly. RSV is the leading cause of respiratory-related hospitalization in young children worldwide and remains a primary cause of hospitalization for infants in the United States.
During the “tripledemic” season of 2022, when RSV cases surged alongside COVID-19 and influenza, intensive care units were inundated with young patients. The cross sectional study, found that some infants required invasive mechanical ventilation, while others received extracorporeal membrane oxygenation. The scarcity of documented monoclonal antibody receipts underscores the need for better prevention strategies.
“In the midst of a triple health crisis, children are confronted with heightened susceptibility to infections, the possibility of healthcare resource shortages, interruptions in routine medical care, as well as psychological and social difficulties,” emphasizes Julie Abrams, associate director of programs and response at Healthcare Ready.
We must prioritize RSV prevention for all infants through initiatives like nirsevimab and the maternal RSV vaccination. Ongoing research will guide recommendations for prophylactic measures and vaccine usage to protect our most vulnerable.
Influenza
Influenza, particularly flu B, keeps many children out of school every year, and this fall, we face an uncertain outlook. Influenza is highly contagious and causes a range of symptoms, and while most children recover, some do not.
The 2022-2023 flu season was one of the earliest and most severe in recent memory. This year, Australia’s flu season, which often precedes the U.S. season, was also significant, indicating a challenging flu season ahead. Regardless of severity, children must receive the flu vaccine to avoid serious illness, as some do succumb to influenza each year.
The seasonal flu shot and maternal vaccination are safe and effective for individuals aged 6 months and older, and timely vaccination can make a significant difference in preventing the spread of this contagious disease. Pregnant women who receive a flu shot are also helping to protect their babies from flu illness for the first several months after their birth, when they are too young to get vaccinated.
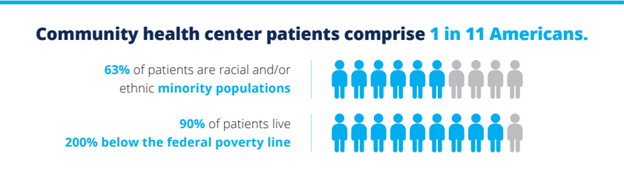
“Being prepared involved giving priority to vaccination efforts, broadening the use of telehealth services, and guaranteeing the availability of mental health assistance to enhance our ability to respond with greater strength and resilience. This also includes planning for increased healthcare capacity, maintaining a stock of pediatric specific supplies and promoting cooperation among different agencies to protect the most vulnerable patients, especially those in lower-income or underserved communities,” says Abrams.
COVID-19
Pediatric COVID-19 cases are on the rise in the wake of in-person schooling, but precise numbers are challenging to ascertain. Hospitalization rates among pediatric patients have not seen a significant increase despite rising cases. Yet, the emergence of new variants like EG.5, F.L.1.5.1, and XBB.1.16 remains a concern, making vaccination even more critical.
Vaccination is the most effective strategy to mitigate the impact of COVID-19, and the CDC recommends updated boosters for children aged 6 months and older. Vaccination is safe and has fewer side effects compared to the disease itself, which can be fatal for children.
As the fall of 2023 unfolds, we must confront the “tripledemic” head-on. It’s time to invest in our children’s health, improve pediatric emergency preparedness, and prioritize their well-being. The consequences of inaction are too grave, and the time for change is now.